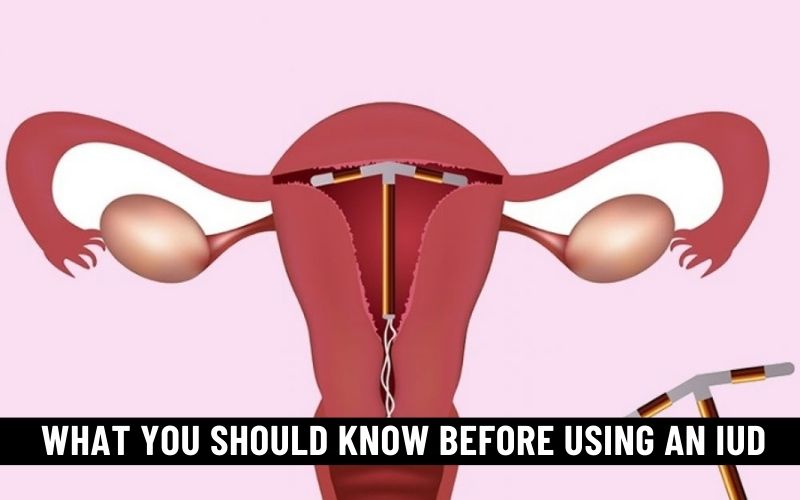
Intrauterine devices (IUDs) have become a popular and highly effective form of contraception for women around the world. These small, T-shaped devices offer a long-term solution to preventing unwanted pregnancies. However, these birth control devices are not without their considerations.
Hence, before you opt for an IUD, there are a few important things that you must keep in mind. Let’s delve into them in detail and help you understand what you’re getting yourself into.
Types of IUDs
The first thing to understand about IUDs is that there are different types available. The two main types are hormonal and non-hormonal (copper) IUDs.
According to Yale Medicine, hormonal IUDs use the hormone progestin to prevent the sperm from reaching the egg. This type of IUD can also make the uterine lining thinner, further inhibiting implantation. Copper IUDs, on the other hand, work by releasing copper ions. These ions are toxic to sperm, which helps prevent fertilization of the egg.
Discuss with your healthcare provider which type is best for you. Hormonal IUDs can also provide relief from heavy menstrual bleeding and painful periods, making them a good choice for women with these concerns. Non-hormonal IUDs don’t contain hormones, which can be appealing to those who prefer hormone-free contraception.
The Insertion Process
Before getting an IUD, you should understand the insertion process. Typically, this is done in a healthcare provider’s office, and it involves a few steps.
The IUD is inserted through the cervix and into the uterus. The process can cause cramping and discomfort, which may persist for a short period afterward. It’s essential to ask your healthcare provider about what to expect during and after the procedure so that you are prepared.
Effectiveness
Healthline affirms the fact that IUDs are one of the most effective forms of birth control available, particularly the hormonal ones. The failure rate is exceptionally low, with fewer than 1 in 100 women experiencing unintended pregnancies within the first year of use.
However, the effectiveness of your IUD also depends on proper insertion and following your healthcare provider’s advice on maintenance.
Also, IUD users must remember that while these devices are highly effective, they don’t protect against sexually transmitted infections (STIs). Therefore, if you are at risk for STIs, continue using barrier methods like condoms in addition to your IUD.
Possible Side Effects
Common IUD side effects include irregular menstrual bleeding, which can range from lighter periods to increased spotting. Some individuals may experience cramping and discomfort, particularly in the initial weeks after insertion, although these symptoms often subside over time.
While IUDs are generally considered safe, there is a rare risk of infection, especially within the first few weeks post-insertion. Besides, IUD expulsion, where the device partially or completely comes out of the uterus, can occur but is relatively infrequent.
Read Also: Best Eye Vitamins Health & Vision and Supplements 2024
More serious but rare side effects may include perforation of the uterus during insertion, which necessitates immediate medical attention. In some cases, hormonal IUDs can lead to hormonal changes that affect mood and skin. However, these side effects are less common than those associated with oral contraceptives.
Another possible hazard to watch out for when using an IUD is breakage during removal. According to TorHoerman Law, this has happened with the Paragard IUD. The non-hormonal Paragard IUD has been found to break during removal, causing serious health complications in the process.
The Paragard lawsuit was filed by the victims of this IUD catastrophe, seeking compensation for their injuries and medical bills. As of September this year, there are over 2,000 cases pending in the Paragard MDL. Over 600 of those cases were filed in 2023 alone.
Duration and Removal
A major advantage of IUDs is their long-lasting protection. Depending on the type, WebMD reports that IUDs can provide contraception for 3 to 10 years, making them a convenient option for many women. However, it’s essential to remember that these devices are not permanent. When the device’s duration expires, or if you decide to discontinue its use, it must be removed by a healthcare provider.
The removal process is typically simpler and less uncomfortable than insertion. Your healthcare provider will gently tug on the IUD strings to pull it out. It’s vital to have the IUD removed by a professional, as self-removal can be risky and should be avoided.
If you want a new IUD inserted after removing the old one, your healthcare provider can often do it in the same appointment. This ensures continuous protection against unintended pregnancy.
Conclusion
As a contraceptive, an IUD is arguably one of the most effective options. However, to ensure maximum effectiveness, you must first understand what you’re getting into. Hence, if you’re planning to opt for IUDs, keep the above-discussed things in mind. Doing so will help you get the most out of these devices while staying cautious of their side effects.